“Gratefulness is the inner gesture of giving meaning to our life by receiving life as gift.”
On Tuesday, November 3rd of this year, the United States elected a new President and I celebrated my 59th run around the sun. I am extraordinarily delighted on both accounts.
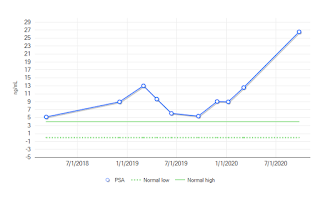
Last month I underwent a full body bone scan and an MRI of the prostate as my physician (Palliative doc in this case) and I attempted to track down what was driving the rapid rise in PSA since the beginning of the year (March - 12.6 ng vs October - 26.6 ng...see previous post).
The best news is that there is zero sign of any bone mets which is the typical metastasis path for PCa cells. It's also one of the most painful complications of the disease. I'm told it's like having multiple compound fractures that hurt 24/7. So this is extremely welcome news.
The not totally unexpected news is that lymph nodes on both left and right have become even more "bulky", having doubled in size since March. Additionally, the extra-capsular extension on the right side is still there to some degree and recurrent disease often occurs at the site of the prior tumor. This MAY be what is happening here and driving the PSA numbers.
In a nutshell, the cancer is active but it's difficult to tell where right now. As a complete cure is not in the cards at this time, I accept that increasing PSA numbers will be part of my future. My hope is simply to be proactive and head off anything like the potential of a cancerous tumor extension invading the bladder or rectum and, currently, there doesn't appear to be any danger of that as was the case last year. Also very good news.
So, relatively speaking, that leaves me doing pretty well for a patient that hasn't followed the majority of his oncologists advice. More precisely, since the end of 2014, the only physician suggested, "Western" treatment that I did follow through on was the 5 session SBRT.
My only other treatment has been high dose cannabis in both oil and flower form with a keen eye on CBD/THC content and ratio. Is this what's kept the beast at bay for as long as it has been? I have no other explanation. I have high/normal testosterone levels which frighten oncologists when it comes to PCa. Other that 2014 and 2019, I've had no standard treatment (i.e. hormone deprivation, surgery, radiation, cryotherapy, etc). The only constant has been cannabis.
So those are the facts currently. But what I want your take away from this post is this. Do I hurt? Oh you betcha; the neuropathy in my feet and hands is relentless and only through pharmacologic intervention am I able to do the amount of walking that I do. The odd pains elsewhere (possible "transference" which is common per the doc) can take my breath sometimes. I try not to bitch about it too much because everyone tires of hearing about it as they can't really see it and I tire of feeling and living with it. How I would love to be able to run like I did before all this. I literally get a visceral jealousy when I see guys closer to my age running.
But I CAN walk! I'm able to work through that. I have Medicare and therefore, I have a wonderful Palliative doc who knows his stuff and my pain is kept pretty tolerable the overwhelming majority of the time.
It would not have been surprising if I'd had urinary difficulty by now. After the SBRT sessions, I did develop some pain and urgency but that has largely subsided and what hasn't is controlled by meds. I read about men who've had the prostate fully removed (an option that makes no sense once the PCa has metastasized...my case) or nuked over 30 or 40 sessions and the horrible, ongoing incontinence and ED they experience.
Although nuked over five, higher dose sessions, I still have some portion of a prostate. I have zero incontinence. I don't ejaculate any liquid to speak of but I DO experience the sensation (aka: dry orgasms....no muss, no fuss?) and erections do happen spontaneous sometimes during the day and are common nocturnally, which is a comforting thing for any 59 year old man. Especially one who has rolled the dice with radiation). Actually, it's a very healthy and comforting thing for a man of any age.
Let me repeat, I have no incontinence issues and sexual function and sensation are quite good. I'll take that as a win!
I'm taking it all as a win! I'm not supposed to be here.......but, I'm still here! Does the Chemo Induced Neuropathic Pain (CINP) get in the way of things and is it chronically painful? Oh yeah; it's like taking the arthritis I already have (can you say part time catering/bartending off and on over 3+ decades?) and compounding it with what we call in Texas, bobwire, and having the wire wrapped around your feet. That's my feet 90% of the time.
Do I get fatigued easily? Oh hell to the yeah. But with planning, I can get what I need to done.
But I'm still here! 7 years in, 2 years more than the estimate IF I did all the docs said I should and 5 more than if I didn't. But, in fairness to them, my case has followed no "usual" course, as I've been told by no less than a dozen physicians of different stripes
Add a little more financial and housing security, warm love of family and friends and far less toxic national news and, well, who knows?!
I'm 59, I'm still here and very grateful for my good fortune!